 | Info
Sheets |
| | | | | | | | | | | | | | | | | | | | | | | | |
 | Out-
side |
| | | | |
|
| | | | | |  | Searchterm 'Frequency' was also found in the following services: | | | | |
|  |  |
| |
|
| |  | | | | | | | | |  Further Reading: Further Reading: | News & More:
|
|
| |
|  |  | Searchterm 'Frequency' was also found in the following services: | | | | |
|  |  |
| |
|
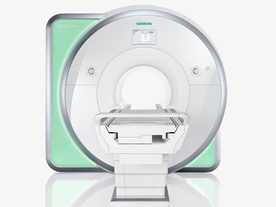
From Siemens Medical Systems;
Received FDA clearance in 2010.
The MAGNETOM Aera is a patient friendly, comfortable 1.5 Tesla MRI system with advanced radio frequency chain.
The system is equipped with the Tim 4G and Dot system (Total imaging matrix + Day optimizing throughput), to enhance both productivity and image quality.
Tim 4G technology provides improved SNR. The standard system configuration of 48 radio frequency channels and 204 coil elements creates an imaging matrix that allows maximum use of coil elements at full field of view. Dot provides improved image consistency through new features like auto align, auto FoV and automatic bolus detection.
Device Information and Specification
CLINICAL APPLICATION
Whole body
Head, spine, torso/ body coil, neurovascular, cardiac, neck, shoulder, knee, wrist, foot//ankle and multi-purpose flex coils. Peripheral vascular, breast, shoulder. Up to 60% more SNR with Tim 4G.
CHANNELS (min. / max. configuration)
48, 64
MINIMUM TE
3-D GRE: 0.22 (256 matrix), Ultra-short TE
At isocenter: L-R 70 cm, A-P (with table) 55 cm
MAGNET WEIGHT (gantry included)
3121 kg
DIMENSION H*W*D (gantry included)
145 x 231 x 219 cm
MAX. AMPLITUDE
33 or 45 mT/m
3 linear with 20 coils, 5 nonlinear 2nd-order
POWER REQUIREMENTS
380 / 400 / 420 / 440 / 460 / 480 V, 3-phase + ground; 85 kVA
| |  | | | |
|  | |  |  |  |
| |
|
•
In the 1930's, Isidor Isaac Rabi (Columbia University) succeeded in detecting and measuring single states of rotation of atoms and molecules, and in determining the mechanical and magnetic moments of the nuclei.
•
Felix Bloch (Stanford University) and Edward Purcell (Harvard University) developed instruments, which could measure the magnetic resonance in bulk material such as liquids and solids. (Both honored with the Nobel Prize for Physics in 1952.) [The birth of the NMR spectroscopy]
•
In the early 70's, Raymond Damadian (State University of New York) demonstrated with his NMR device, that there are different T1 relaxation times between normal and abnormal tissues of the same type, as well as between different types of normal tissues.
•
In 1973, Paul Lauterbur (State University of New York) described a new imaging technique that he termed Zeugmatography. By utilizing gradients in the magnetic field, this technique was able to produce a two-dimensional image (back-projection). (Through analysis of the characteristics of the emitted radio waves, their origin could be determined.) Peter Mansfield further developed the utilization of gradients in the magnetic field and the mathematically analysis of these signals for a more useful imaging technique. (Paul C Lauterbur and Peter Mansfield were awarded with the 2003 Nobel Prize in Medicine.)
•
1977/78: First images could be presented.
A cross section through a finger by Peter Mansfield and Andrew A. Maudsley.
Peter Mansfield also could present the first image through the abdomen.
•
In 1977, Raymond Damadian completed (after 7 years) the first MR scanner (Indomitable). In 1978, he founded the FONAR Corporation, which manufactured the first commercial MRI scanner in 1980. Fonar went public in 1981.
•
1981: Schering submitted a patent application for Gd-DTPA dimeglumine.
•
1982: The first 'magnetization-transfer' imaging by Robert N. Muller.
•
In 1983, Toshiba obtained approval from the Ministry of Health and Welfare in Japan for the first commercial MRI system.
•
1986: Jürgen Hennig, A. Nauerth, and Hartmut Friedburg (University of Freiburg) introduced RARE (rapid acquisition with relaxation enhancement) imaging. Axel Haase, Jens Frahm, Dieter Matthaei, Wolfgang Haenicke, and Dietmar K. Merboldt (Max-Planck-Institute, Göttingen) developed the FLASH ( fast low angle shot) sequence.
•
1988: Schering's MAGNEVIST gets its first approval by the FDA.
•
In 1991, fMRI was developed independently by the University of Minnesota's Center for Magnetic Resonance Research (CMRR) and Massachusetts General Hospital's (MGH) MR Center.
•
From 1992 to 1997 Fonar was paid for the infringement of it's patents from 'nearly every one of its competitors in the MRI industry including giant multi-nationals as Toshiba, Siemens, Shimadzu, Philips and GE'.
| | | |  | |
• View the DATABASE results for 'MRI History' (6).
| | |
• View the NEWS results for 'MRI History' (1).
| | | | |  Further Reading: Further Reading: | | Basics:
|
|
News & More:
| |
| |
|  |  | Searchterm 'Frequency' was also found in the following services: | | | | |
|  |  |
| |
|
The subacute risks and side effects of magnetic and RF fields (for patients and staff) have been intensively examined for a long time, but there have been no long-term studies following persons who have been exposed to the static magnetic fields used in MRI. However, no permanent hazardous effects of a static magnetic field exposure upon human beings have yet been demonstrated.
Temporary possible side effects of high magnetic and RF fields:
•
Varying magnetic fields can induce so-called magnetic phosphenes that occur when an individual is subject to rapid changes of 2-5 T/s, which can produce a flashing sensation in the eyes. This temporary side effect does not seem to damage the eyes. Static field strengths used for clinical MRI examinations vary between 0.2 and 3.0 tesla;; field changes during the MRI scan vary in the dimension of mT/s. Experimental imaging units can use higher field strengths of up to 14.0 T, which are not approved for human use.
•
The Radio frequency pulses mainly produce heat, which is absorbed by the body tissue. If the power of the RF radiation is very high, the patient may be heated too much. To avoid this heating, the limit of RF exposure in MRI is up to the maximum specific absorption rate (SAR) of 4 W/kg whole body weight (can be different from country to country). For MRI safety reasons, the MRI machine starts no sequence, if the SAR limit is exceeded.
•
Very high static magnetic fields are needed to reduce the conductivity of nerves perceptibly. Augmentation of T waves is observed at fields used in standard imaging but this side effect in MRI is completely reversible upon removal from the magnet. Cardiac arrhythmia threshold is typically set to 7-10 tesla. The magnetohydrodynamic effect, which results from a voltage occurring across a vessel in a magnetic field and percolated by a saline solution such as blood, is irrelevant at the field strengths used.
The results of some animal and cellular studies suggest the possibility that electromagnetic fields may act as co-carcinogens or tumor promoters, but the data are inconclusive.
Up to 45 tesla, no important effects on enzyme systems have been observed. Neither changes in enzyme kinetics, nor orientation changes in macromolecules have been conclusively demonstrated.
There are some publications associating an increase in the incidence of leukemia with the location of buildings close to high-current power lines with extremely low- frequency (ELF) electromagnetic radiation of 50-60 Hz, and industrial exposure to electric and magnetic fields but a transposition of such effects to MRI or MRS seems unlikely.
Under consideration of the MRI safety guidelines, real dangers or risks of an exposure with common MRI field strengths up to 3 tesla as well as the RF exposure during the MRI scan, are not to be expected.
For more MRI safety information see also Nerve Conductivity,
Contraindications, Pregnancy
and Specific Absorption Rate.
See also the related poll result: ' In 2010 your scanner will probably work with a field strength of' | |  | |
• View the DATABASE results for 'MRI Risks' (9).
| | |
• View the NEWS results for 'MRI Risks' (3).
| | | | |  Further Reading: Further Reading: | Basics:
|
|
News & More:
| |
| |
|  |  | Searchterm 'Frequency' was also found in the following services: | | | | |
|  |  |
| |
|

It is important to remember when working around a superconducting magnet that the magnetic field is always on. Under usual working conditions the field is never turned off. Attention must be paid to keep all ferromagnetic items at an adequate distance from the magnet. Ferromagnetic objects which came accidentally under the influence of these strong magnets can injure or kill individuals in or nearby the magnet, or can seriously damage every hardware, the magnet itself, the cooling system, etc..
See MRI resources Accidents.
The doors leading to a magnet room should be closed at all times except when entering or exiting the room. Every person working in or entering the magnet room or adjacent rooms with a magnetic field has to be instructed about the dangers. This should include the patient, intensive-care staff, and maintenance-, service- and cleaning personnel, etc..
The 5 Gauss limit defines the 'safe' level of static magnetic field exposure. The value of the absorbed dose is fixed by the authorities to avoid heating of the patient's tissue and is defined by the specific absorption rate.
Leads or wires that are used in the magnet bore during imaging procedures, should not form large-radius wire loops. Leg-to-leg and leg-to-arm skin contact should be prevented in order to avoid the risk of burning due to the generation of high current loops if the legs or arms are allowed to touch. The patient's skin should not be in contact with the inner bore of the magnet.
The outflow from cryogens like liquid helium is improbable during normal operation and not a real danger for patients.
The safety of MRI contrast agents is tested in drug trials and they have a high compatibility with very few side effects. The variations of the side effects and possible contraindications are similar to X-ray contrast medium, but very rare. In general, an adverse reaction increases with the quantity of the MRI contrast medium and also with the osmolarity of the compound.
See also 5 Gauss Fringe Field, 5 Gauss Line, Cardiac Risks, Cardiac Stent, dB/dt, Legal Requirements, Low Field MRI, Magnetohydrodynamic Effect, MR Compatibility, MR Guided Interventions, Claustrophobia, MRI Risks and Shielding. | | | | | | | | |
• View the DATABASE results for 'MRI Safety' (42).
| | |
• View the NEWS results for 'MRI Safety' (13).
| | | | |  Further Reading: Further Reading: | Basics:
|
|
News & More:
| |
| |
|  | |  |  |
|  | | |
|
| |
 | Look
Ups |
| |